|
WE’RE RE-OPENING!!!
We are so excited to let everyone know that we are reopening as of Monday May 4, 2020. Feel free to call the clinic and we’ll be happy to book your appointment! But before you do, please read below to see what will be expected of you and what kind of changes we’re making to keep you safe!
Why are we asking you to wear a face covering? Well, this is something we’re asking you to do to protect the staff and the other clinic patients with whom you may come in contact. If you happen to be an unknowing asymptomatic carrier, any of your coughs or sneezes will be kept more contained by your mouth and nose covering. What will we as staff be wearing you may wonder? We will be wearing our regulatory college sanctioned disposable face masks, and some staff may be wearing eye shields.
Have you or anyone in your household travelled outside of Manitoba in the past 14 days? Have you or anyone in your household been in a setting that has been identified as a risk for acquiring COVID-19, such as at a workplace or an event in the past 14 days? Have you or anyone in your household been in contact with someone that is confirmed to have COVID-19 in the last 14 days? Have you or anyone in your household had laboratory exposure while working directly with specimens known to contain COVID-19? Have you or anyone in your household been recommended or instructed to self isolate in the past 14 days? Do you have a new onset of any of the symptoms listed below: Fever Cough Sore Throat Shortness of breath/breathing difficulties Do you have new onset of 2 or more of any of the symptoms listed below: Runny nose Muscle aches Fatigue Loss of taste or smell Headache Hoarse voice Nausea, vomiting, or diarrhea for more than 24 hours You can find a COVID self screening tool at this link if you would like to self screen as well: https://sharedhealthmb.ca/covid19/screening-tool/ If you’ve answered yes to any of the screening questions above and you are concerned that you may require COVID testing, please call Health Links at: 204-788-8200 or 1-888-315-9257.
Anyone who has answered yes to any of the questions above. In this case, we would help you to arrange a virtual session with one of our physios.
In this case, we would help you to arrange a virtual session with one of our physios.
Limiting the number of people in the clinic to a maximum of 10 at a time, including staff. Having everyone sanitize their hands immediately upon entering the clinic. Practicing social distancing (staying 6 feet apart) whenever possible. Avoiding having people wait in the wait room and removing all public magazines, books, and pamphlets. We normally clean all of our beds and bolsters, change pillowslips, and sanitize the gym between patients but don’t be surprised if you start smelling industrial strength sanitizer everywhere you go! Our therapists normally ensure they sanitize their hands between patients and before invasive procedures like acupuncture, but as described above, you can be sure it’s happening stringently just by the smell! Ensuring our own staff are screened as above and are monitoring themselves for any signs of symptoms so they STAY HOME if they are ill. We thank you for adjusting with us to this new way of keeping you healthy at the clinic. I know there will be some bumps and laughs along the way … we’ll all have fun trying to guess who is who and trying to hear each other’s muffled words behind our mouth coverings! In the end, we just want to keep you and your loved ones safe while still helping you along in your healing process. So excited to see you at the clinic! CORONAVIRUS: COVID-19 “Stock Up On Information, Not Toilet Paper” That is a direct quote from Manitoba’s chief public health officer Dr. Brent Roussin and couldn’t be more true. There are a lot of questions being asked (rightly so) and unfortunately a lot of inaccurate responses going around. Here are some FACTS about COVID-19 that have been discovered as of March 13, 2020:
COVID-19 is a disease that affects your respiratory system by causing viral infections in your nose, throat, and lungs.
Pandemic refers to the geographic location and the speed of transmission of a disease, not to the severity of a disease. A pandemic refers to a disease that has spread over a large geographic area, usually including international borders, relatively quickly. The word pandemic does not mean that the disease will have severe symptoms in all of the people who become infected. What do people mean when they use the word “quarantine”? There is the generalized use of the term “quarantine” where you don’t have the virus but voluntarily want to keep yourself at home to avoid getting the virus. Then there is the type of quarantine we refer to as “self isolation” when you are ill with the virus (or suspected ill with the virus) and your doctor tells you not to leave the home unless necessary. For more information on self isolation, see: https://www.gov.mb.ca/health/publichealth/factsheets/coronavirus_selfisolation.pdf This is not the same as a “lock down”, where the government makes it a law that you have to stay in your homes at all times. Why do we quarantine? It is all about slowing the spread of the virus. It’s about preventing everyone from becoming sick all at once and for those who do become ill and need hospital care (only about 20% of people who get the virus will need this), not overwhelming the health care system so we have hospital beds in which to put these sick people.
Some studies have found the virus in blood, urine and feces but the jury is still out on whether these fluids can be a form of transmission of the disease.
Short answer: No Longer answer: Infection control specialists differentiate between diseases that can travel through the air briefly on droplets and diseases that aerosolize and float around in the air for longer periods. If a virus floats around in the air for longer periods in a concentrated form that you can breathe in and contract, it is considered an “airborne” virus. COVID-19 is not currently considered an airborne virus. Even longer answer: This virus is new, and we haven’t been able to study it for very long. One study that looked at the persistence of coronaviruses in general reported that these viruses could live up to 4 days on wood, 5 days on metal, paper, and glass, and 9 days on plastic. https://www.journalofhospitalinfection.com/article/S0195-6701(20)30046-3/fulltext Another recent study (that has not yet been peer reviewed or officially published) has looked at how long COVID-19 could survive on different surfaces after shaking the virus up in a machine and aerosolizing it. It was found that the virus may be able to live in the air for up to 3 hours, on copper for up to 4 hours, on cardboard for up to 24 hours, and on stainless steel and plastic for up to 3 days after being aerosolized in that machine. https://www.scribd.com/document/451558810/COVID-Surface-study#from_embed That doesn’t mean that this virus has an airborne transmission. This virus is currently believed to be transmitted by droplets, contaminated hands, and surfaces. So you need to touch a surface that has been contaminated and not cleaned and then touch your mouth, nose, or eyes, or be within 6 feet of someone who has sneezed or coughed and then directly breath the droplet in through your mouth or nose. In Singapore, the air was sampled in hospital rooms occupied by patients with COVID-19 and the virus was not found in the air. https://jamanetwork.com/journals/jama/fullarticle/2762692
Wash/sanitize your hands regularly and thoroughly and try not to touch your face. FYI for those of you who love stats as much as I do: Just how often do I really touch my face? In one observational study, students were noted to touch their face 23 x per hour!! (Kwok, Y.L., Gralton, J., and McLaws, M.L. Face touching: a frequent habit that has implications for hand hygiene. Am J Infect Contr. 2015; 43: 112–114) Practice “social distancing”. Wipe down/sanitize surfaces that are commonly used like public computer keyboards or countertops or your cell phone. Avoid directly touching objects that are commonly known to be dirty like using a paper towel to open bathroom doors or using your knuckle to hit the button on the elevator or a public light switch. Stay home if you don’t feel well. Avoid non essential travel outside of the city.
However, it is still important to take any antibiotics your doctor has prescribed to you to treat other infections you have and to get the flu shot to prevent other viral illnesses.
As of March 13, 2020, Manitoba Health is directing people who have these symptoms to call Health Links –Info Sante and they will help to determine your next steps. Health Links: (204) 788-8200 OR 1-888-315-9257. They are open 24 hours a day, 7 days a week. If they feel you need to be tested for COVID-19, they will direct you to a community screening location (usually at one of the ACCESS centres). https://news.gov.mb.ca/news/?archive=&item=46930 If it is an emergency because you cannot breathe, call 911 as you would normally. This link will direct you to the Manitoba Government’s latest bulletins: https://www.gov.mb.ca/health/
Approximately 20% of people who get the virus will need to be hospitalized for medical care – these tend to be people who are over the age of 65 and have other comorbidities (other illnesses), or those with compromised immune systems. So what should I do? Stay at home as much as you can and avoid having unnecessary visitors to try and avoid spreading the disease. It’s Netflix time, baby!
That it is important to take this virus seriously, but not to panic. Wash your hands and try not to touch your face. For more information on COVID-19, make sure to look for reputable sources such as the Government of Manitoba health sites: https://www.gov.mb.ca/health/coronavirus/public.html Not the panic and buy all the toilet paper and Tylenol sites. 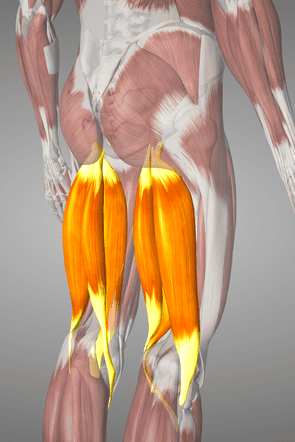 What are the Hamstrings? The hamstring muscles are a group of 3 muscles located at the back of your thigh called Biceps femoris, Semimembranosus and Semitendinosus. Biceps femoris is the largest of the hamstrings and the one that gets injured most often. All three muscles begin from a part of your pelvic bone called your ischial tuberosity (or sit bone as it is sometimes referred to) and attache to the upper part of the two long bones in your lower leg, the tibia and the fibula. What do the Hamstrings do? The hamstrings are a two joint muscle crossing both the hip and knee. They have two main actions: extending the hip (bringing the whole leg back) and bending the knee. This means that your hamstrings are active when you come up from a squat, get ready to kick a soccer ball, and even just while walking. How can the Hamstrings get injured? There are two commons ways that your hamstrings can be injured:
What are the signs and symptoms of a Hamstring injury? The following non-exhaustive list presents typical signs and symptoms of a hamstring injury:
What are the risk factors for Hamstrings injury?
How long does it take to heal? Healing time depends on the mechanism, location, size, and severity of the Hamstring injury. It also varies widely from person to person. Your physical therapist or medical doctor can assess your injury and provide an estimated healing time with appropriate activity restrictions. Return to play or work are based on the specific tasks and demands required of you. Your physical therapist can tailor your rehabilitation program to fit your work and/or sport. The physiotherapy approach to rehabilitating Hamstring injuries Your physiotherapist will take a thorough history and conduct a comprehensive physical exam before treating your injury. In some cases, physiotherapy may not be appropriate and you will be referred to the appropriate healthcare provider by your therapist. Physiotherapy is a client centered medical profession and incorporates your goals into the rehabilitation program. The ultimate goals of physical therapy are to return to your pre-injury level of function free of pain, and to minimize the risk of re-injury. You and your therapist will decide on the treatment choices according to the specifics of your injury, current evidence based research, and your response to the treatments. Your therapist may offer some of the following treatments options:
Education regarding your injury such as your diagnosis, prognosis, self-care, and prevention of re-injury are always an important part of your care. If you suspect you may have an injury or are looking to prevent an injury, come on in and we’ll take a look! Written by: Binudith Warnakulasooriya, Masters of Physical Therapy Student Edited by: Andrea Giacobbo BScPT, BA References Baheti, N. D., & Jamati, M. K. (2016). Physical therapy treatment of common orthopedic conditions. New Delhi: Jaypee Brothers Medical (P) Ltd. 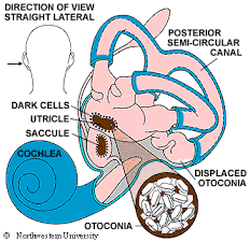 BPPV This stands for Benign Paroxysmal Positional Vertigo. Benign – not life threatening and not progressive Paroxysmal – sudden attacks, commonly with no initial cause Positional – triggered by head position changes Vertigo – spinning sensation It is the most common vestibular disorder and is curable 80-98% of the time!
 Shovelling snow is hard work!! It requires strenuous use of your arms, legs, back and heart. Add in cold weather that causes your muscles and blood vessels to tighten up, makes it harder to breathe, and requires the body to work harder to regulate its internal temperature and you’ve got an incredibly intense workout on your hands. For people who are physically fit enough to handle the task, this is as good of a workout as jogging. For those who aren’t prepared for this type of activity, injuries are common. We see a lot of rotator cuff strains (sore shoulders), back strains, and even heart attacks this time of year. Repetitive twisting, improper lifting, and lack of aerobic conditioning are the biggest causes of injuries when it comes to snow shovelling.
|
AuthorPhysiotherapists of Seine River Physiotherapy Archives
May 2020
Categories |
|
We are located on the 2nd floor of the Seine River Professional Center, on St. Anne's Rd just south of Abinojii Mikanah (Bishop Grandin Blvd) and are wheelchair accessible.
Address: 600 St Anne's Rd #220, Winnipeg, MB R2M 2S2 Phone: (204) 415-5006 |

Copyright 2024
Seine River Physiotherapy |


 RSS Feed
RSS Feed